
What is a concussion?
According to the Webster 20th Century dictionary (1938) a concussion is defined as the act of violently shaking or agitating by the stroke or impulse of another body. This derives from the Latin n. concussio, a violent shock, vt coculere to shake violently. The term concussion in a medical context is often referred to as mild traumatic brain injury, mTBI. These terms are often used interchangeably, but both refer to the transferal of sufficient energy to the brain from a blow to the head to result in well described symptoms such as loss of consciousness, acute confusion, headache, listlessness and insomnia. No universally accepted definition for concussion/mTBI exists at this writing. Several definitions for mTBI have been proposed by various organizations including the American Congress of Rehabilitation Medicine (ACRM), Center for Disease Control and Prevention (CDC), the World Health Organization (WHO) and the Department of Defense (DOD). On the other hand, the American Academy of Neurology (AAN) and the Concussion in Sport Group (CISG) have proposed definitions for concussion.
According to the AAN, a concussion is defined as ”a trauma-induced alteration in mental status that may or may not involve loss of consciousness.” In this definition confusion and amnesia are cardinal manifestations of concussion and generally occur immediately after the blow to the head. In any case, a blow to the head results in either an acute acceleration or deceleration of the brain which produces an injury from a complex yet stereotypically patterned process. The precise details of the effects which result from a concussion are not completely understood.
CISG defines mTBI as traumatically induced functional disruption of brain physiology manifested by at least one of the following:
- Any loss of consciousness;
- Any loss of memory for events immediately before or after the accident;
- Any alteration in mental status at the time of the accident (e.g. feeling dazed, disoriented or confused);
- Focal neurological deficit or deficits that may or may not be transient
The severity of the injury may not exceed the following:
- Loss of consciousness of approximately 30 minutes or less;
- After 30 minutes, an initial Glasgow Coma Scale (GCS) score of 13-15; and
- Posttraumatic amnesia (PTA) not lasting greater than 24 hours
As stated previously there is not universal agreement regarding these definitions. For example, when should one consider any injury to the brain to be minor? In my view, the crux of a concussion/mTBI results from the transmission of energy from one body to the next. In case of the brain this results in transient or permanent alteration in how this organ functions. Further, it is increasingly recognized that sub-concussive, i.e. those which produce no evident symptoms, blows to the head may result in long-term alteration of cognitive function. In other words, any occupation which may result in what might otherwise be considered repeated trivial blows to the head can result significant and permanent brain injury. Any single such impact has no outward or evidence of affect, but the cumulative effect of many such impacts may well alter brain function over the long-term. This has very serious implications with respect to contact sports in particular. Going forward, I will use the term traumatic brain injury (TBI) to include any injury to the head that may or may not result in loss of consciousness, but results in evident alteration of brain functioning or any such injury which may have the potential to impair brain functioning over time.
TBI: How much of a problem is it?
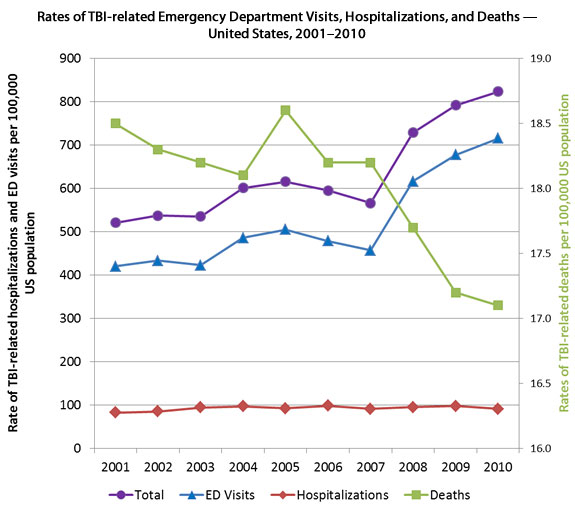
According to the CDC, TBI accounted for nearly 2.7 millions hospitalizations, ED visits and deficits in 2010. This compares to 1.7 million in 2001 which is illustrated in the figure below as rate per 100,000 population.
Evidence from numerous sources from multiple countries has indicated a very strong correlation between repeated head injury from any cause and neurodegenerative disorders. Such degenerative processes have been described in boxers who are at risk for developing dementia, dementia pugilistica, the first report of which occurred in 1954. This 51-year-old retired boxer had antemortum symptoms of dementia and personality changes and pathological brain changes of Alzheimer’s disease at autopsy. Soccer players may be at risk for both dementia and amytrophic lateral sclerosis (ALS). Recent evidence correlates lifetime exposure to headers and long-term risk of ALS in soccer players. Professional football players have been found to be at risk for an entity known as chronic traumatic encephalopathy (CTE). Multiple studies have shown cognitive decline in many other contact sports such as ice hockey, karate, rugby and lacrosse. Genetic predisposition may play an important role in the individual susceptibility to these conditions.
While cognitive and behavioral changes in former NFL players had been known for years, the first report of neuropathological changes of the brain of a retired NFL player were described by Omalu et al in 2005 in Neurosurgery. The subject played for 17 seasons in the NFL from the age of 22 until he retired at the age of 38. He also played football in both high school and college as is true for most NFL players. He displayed behavioral changes such as anxiety and depression as well as problems with memory and judgement according to family members. In this report, Dr. Omalu found changes in the player’s brain similar, but not identical to those found in persons with Alzheimer’s disease. This pattern of pathological findings of the brain, which have been described in multiple former NFL players, are now referred to as chronic traumatic encephalopathy or CTE.
In 2013 approximately 2.8 million TBI incidents occurred in the United States. It is likely the leading cause of death in people under the age of 24 years. What is more, it is a prevalent cause of long-term disability which results in a substantial drain on public and private finances. No specific medical remedy exists for restoring or even improving brain function following TBI. Treatment focuses on removing the participant from risk of further head injury at least until all symptoms of concussion have subsided. The most prevalent causes of TBI are falls, motor vehicle accidents and personal violence which includes participation in contact sports. Blast/explosive-induced injuries are common in military personnel. Repeated head injury of any cause may increase the long-term risk of Alzheimer’s disease.
The CDC has estimated that between 1.6 and 3.8 million sports-related concussive injuries occur annually in the United States accounting for approximately 5–9% of all sports-related injuries. Approximately 1.1 million students participated in American high school football in 2008-09. Estimates indicate that from 43,000 to 67,000 such players are diagnosed with concussion. That said, it is likely that a large proportion of sports-related concussions escape diagnosis. Reasons for these participants not being diagnosed may include general ignorance of the serious consequences associated with concussion and fear of being held out of competition to say nothing of concern over loss of future income. The total number of concussions in younger players is even higher due to the higher number of participants. Further, younger individuals are likely more susceptible to the effects of repeated mTBI.
Associated conditions such as ADD, learning disability, migraine, female gender and specifics of the sport itself probably confer added risk for concussion and/or prolonged effects from concussion. Importantly, a history of prior concussion increases the risk of having future concussions and persistent symptoms following a concussion.
Even more concerning than the student athlete who fails to report covert symtoms of concussion e.g. headache and insomnia, are those who experience multiple blows to the head, have no symptoms yet are at risk for brain injury. Such head impacts are now known as subconcussive and are much more frequent than concussive injuries. Research has demonstrated that such impacts probably occur hundreds of times over the course of a typical high school football season
In 2014 researchers from Purdue University reported on the outcomes of 11 high school football players who wore helmets fitted with accelerometers designed to record significant collision events during both practice and games. These players all had a pre-season baseline neurocognitive evalution and functional MRI (fMRI) to assess the brain’s neurophysiological connectivity during a visual memory test. Selected players with (1) diagnosed concussion, (2) no concussion, but a high number of collision events indicated by the accelerometers or (3) neither concussion nor high number of collision events had follow up in season and post season re-assessments As expected, all players who were diagnosed with a concussion had significant deterioration of performance on the cognitive testing and changes on fMRI.
Unexpected were findings of cognitive decline and changes in brain physiology as demonstrated by fMRI in half of the players not diagnosed with concussion. All of these players had a high number of collision events overall, but particularly higher energy events (>80g) to the top front portion of the helment which overlies an area of the brain thought to be critical to the functioning of working memory. Other similar studies suggest that a substantial proportion of participants in such sports are at risk for long term brain injury from blows to the head that typically fly below the radar of medical personnel.
Because of the results of such research, some clinical professionals have suggested that head impact data be included as standard equipment for football players at all levels. Others have recommended that tackle football not begin before the age of 14 or 15 years. Additionally, these data may be used by coaches or other training staff to track the pattern of impacts which may then be used to modify practice sessions for improved coaching techniques especially with respect to blocking and tackling. One unexpected results of research comparing high school football players to collegiate ones is that the latter appear to experience far fewer head impacts compared to their younger cohorts.
What to do?
The first step is to identify players who are experiencing deterioration of brain functioning whether overt or covert. A large part of this should now involve the recognition of the potentially deleterious effects of sub-concussive impacts. Many players with concussions do not come to medical attention which suggests that all participants with sub-concussive head impacts escape detection. Ideally, all prospective participants in contact sports such as football should be evaluated with baseline neurocognitive testing before the season begins. A simple CPT test such as QIK (http://www.eeginfo.com/qiktest/cpt_qiktest.pdf) is appropriate and has a large database from which players may be compared to normal subjects. This test evaluates executive function, sensory processing, motor control, focused attention, processing speed, impulsivity and consistency of brain functioning. In other words, it interrogates brain functioning in a sweepingly broad manner which reflects the integrity of the nervous system as a whole. The test takes about 21 minutes and is very easy to administer. It is not subject to practice effect. Players could then undergo in season and post season testing to check for any deterioration in performance. Such information provides objective, actionable data regarding cognitive functioning.
Monitoring the number and severity of head impacts which occur during practice and games as researchers at Purdue and the University of North Carolina have done may not be feasible for many high school programs, but it is available. Such studies may lead to changes in coaching techniques and recommendations on the evaluation and management of participants who demonstrate a decline in neurocognitive performance. Moreover, such information along with that from neurocognitive testing can provide reliable data upon which coaching and medical staff can make rational decisions about whether a players should practice, play or undergo further medical evaluation. As indicated above, there is ample evidence that sub-concussive impacts can lead to long-term cognitive dysfunction.
Current cognitive rehabilitation and other conventional therapies for mTBI are inadequate in terms of restoring patients to a prior level of functioning. Neurofeedback has been used for many years in persons with head injury of various causes. Some of the earliest descriptions of improvement in symptoms from head injury treated with NF are 30 years old. All studies report significant improvement in subjective symptoms and/or objective cognitive testing. Symptomatic improvement was seen in attention, impulse control, judgment and processing speed. Neurofeedback avoids side effects inherent with medications and has been shown to have lasting effects. It literally assists the brain in healing itself rather like a pathfinder. Further, rather than soley using neurofeedback as a responsive therapy only, one may consider using it preemptively to mitigate the effects of concussive and sub-concussive brain injury.
For more information about how Neurofeedback can help you, contact us at info@4amentaledge.com

